Arthrosis is a disease that is characterized by the gradual destruction of the joint due to the development of dystrophic changes in the tissues.According to the WHO, every tenth resident of the planet is confronted with this problem.After 50 years, the risk of the occurrence of the disease is about 30%and reaches 80 to 90%.
General information
Arthrosis is a chronic, long -term process that not only affects joints.During progress, dystrophic and degenerative changes are surprisingly the auxiliary apparatus.The patient is with inflammation of the cartilage and the bone tissue, the capsule of the joint and periosemantial bag as well as the muscles, ligaments and subcutaneous tissue that come into contact with them.
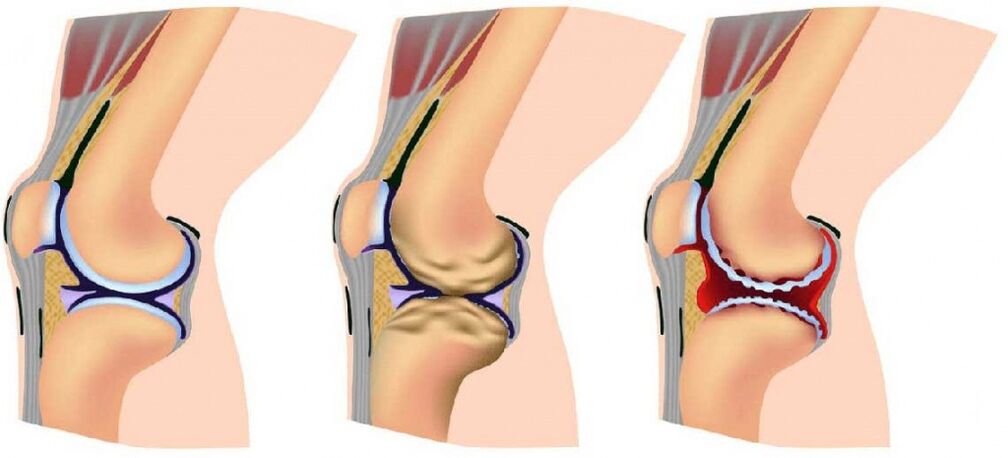
Regardless of the localization, the pathological process flows according to a single scheme.First, the balance between the growth processes and the destruction of the cartilage is disturbed in the thickness of the substance and the balance is shifted in favor of dystrophy and reverse development (degeneration).At this point, the changes for the eye occur in the microstructure of the cartilage, which leads to its thinning and cracks.
In the course of the disease, the joint loses its elasticity and becomes denser.This reduces its ability to depreciate, the speed of tissue damage is constantly increasing during the movements due to vibrations and microtrauma.The thinning of the cartilaginous layer provokes the active growth of bone structures, which means that spikes and runners develop on the smooth surface of the joint - osteoarthrosis.Movements are becoming increasingly limited and painful.Cramps of the muscles that surround the affected area develops what makes the pain worse and deforms the limb.
Disease stages
The arthrosis of the joints gradually develops and in the process three consecutive stages that determine the severity of the disease:
- Level 1: The pathology is not found on an X beam or an ultrasound, but the destruction processes have already been started.The composition of the joint fluid changes, whereby the tissue is maintained less than nutritious creatures and becomes more sensitive;The increased stress on the damage area causes inflammation (arthritis) and pain;
- The 2nd stage is characterized by the active destruction of cartilage tissue, and bone spikes and growth appear along the edges of the common platform (contact area of surfaces).At this point, the pain becomes familiar and inflammatory processes become stronger or weaker.Cramps associated with the joint of the muscles are regularly noted;
- Stage 3: The destructive areas affect almost the entire surface of the cartilage, the joint platform is deformed, the injured member deviates from its axis;The movement volume is reduced and the ligaments weaken and become short.
Some experts also differentiate between the IV development stage of osteoarthritis.It is characterized by an almost complete immobility of the joint.
Guy
Depending on the cause of the disease, primary and secondary arthrosis are differentiated.In the first case, the pathology arises regardless of the background of a comprehensive effect of predisposing factors.The secondary form is the result of other diseases and is divided into the following groups:
- Damage to the joints that occurred due to metabolic disorders or endocrine diseases (gout, diabetes mellitus, acromegaly, hyperparathyroidism);
- Destruction in connection with congenital pathologies (pedget disease, congenital lip injury, scoliosis, hemophilia, etc.);
- Post -Traumatic arthrosis that arose against the background of fractures, cracks, necrotic processes or surgical operations and arise due to the characteristics of the profession.
The most sought -after classification of osteoarthritis, depending on the localization of the pathological process:
- Gonar rose: the lesion of the knee, one of the varieties, their palet pemory arthrosis -is the destruction of the joint between the thigh bone and the patella;
- Osteoarthritis of the ankle joint: occurs against the background of a large burden and frequent injuries;
- Osteoarthritis of the footpaths: The thumb most often suffers from the intersection with the foot;The defeat develops against the background of the gout or valgus deformation;
- Shoulder arthrosis is characterized by damage to the shoulder and is often found at a young age against a background of increased physical activity (makers, athletes, builders).
- Coksartrose: damage to the hip joint;Perhaps both a -siucian and bilateral and is one of the frequent causes of disabilities in people over 50;
- The destruction of the cartilaginous slices between the vertebrae most often influences the neck and lumbar spine;
- Arthrosis of the joints of the brush: the finger connections are most often affected, the pathologies are particularly susceptible to women in menopause.
- Arthrosis of the temporomandibular joint: it is quite rare, mostly against the background of chronic inflammation due to bite disorders or improper prosthetics;
- Arthrosis of the elbow joint: a rare form of the disease, which is most often associated with violations of this area.
The reasons for the development
The main factor in the development of osteoarthritis is the false adjustment between the test and the joint capacity of the joint to withstand this load.In acute or chronic, this process inevitably leads to the destruction of tissues.
The list of causes that increase the arthrosis risk of localization includes:
- Inheritance;
- Endocrine pathology (diabetes);
- Injuries to the joint apparatus: bruises, transfers, fractures or bone cracks in the joint bag, complete or partial refraction of ligaments that penetrate the wounds;
- Regular increased joint load in connection with the profession;
- Obesity;
- Settlement;
- Transfer inflammatory joint diseases: acute arthritis, tuberculosis, etc.;
- Blood diseases in which bleeding often occur in the joint (hemophilia);
- sharp changes in the hormonal background (pregnancy, menopause);
- Local circulatory disorders in connection with atherosclerosis, varicose veins, thrombophlebitis, etc.;
- Autoimmune diseases (rheumatoid arthritis, systemic lupus erythematodes etc.);
- Dyplasia of connective tissue (congenital pathology, accompanied, including excessive mobility of the joints);
- Congenital pathologies of the musculoskeletal system (flat feet, dysplasia or congenital failure of the hip joint, etc.);
- Age over 45 to 50 years (risk increase is associated with a decrease in collagen synthesis);
- Osteoporosis (bone vacuum);
- Chronic poisoning of the body (including salts of heavy metals, drugs, alcohol);
- Surgical interventions on the joints.
Symptoms
Arthrosis symptoms regardless of their cause and localization, since the changes in the joints are according to the same scenario.The disease develops gradually and begins to manifest when the cartilage is very badly damaged.
One of the first signs of a functional disorder is crunch in the problem area during movement.It usually occurs when the knee or shoulder is damaged.At the same time, after a long inactivity in the morning, a person can feel slight mobility after a long inactivity.
When asked what symptoms occurred with osteoarthritis, most patients first call up pain.At first insignificant and weak, gradually it gains strength and prevents it from moving normally.Depending on the phase and the localization of the pathology, one person can feel:
- Starting pain: occur during the first movements after a long inactivity of the joint and are connected to the formation on the surface of the cartilage of the thin film from the destroyed fabric.After the start of the work, the film shifts and the discomfort disappears;
- Pain with longer physical exertion (standing, walking, running, etc.): It appears due to a decrease in the shock absorption properties of the joint;
- Weather pain: provoked by low temperature, air humidity, atmospheric pressure changes;
- Night pain: combined with venous stagnation and increased blood pressure in the bones;
- Joint blockade: sharp, severe pain in connection with a violation of a cartilage or bone in the joint cavity.
When arthrosis develops, the symptoms become conspicuous so that the patient determines the following signs:
- an increase in morning stiffness;
- Strengthening and increasing the period of pain;
- Acceptance of mobility;
- Joint deformation due to bone growth;
- Deformation of bones and surrounding tissues: The process is clearly recognizable by the limbs and fingers of the hands, which are noticeably curved.
When the inflammation is paved, the affected area swells, blushed and gets hot for touch.If you are pressed on it, the pain increases significantly.

Analyzes and diagnostics
The diagnosis of arthrosis is involved in the orthopedic doctor.He carries out a detailed overview of the patient to identify symptoms and anamnesis.The doctor in detail about the time of the first sign and speed of their development, injuries and illnesses, the presence of similar problems with relatives.
A general blood test enables you to identify an inflammatory process that is often associated with osteoarthritis.
The main method of diagnosis is radiography.The following signs are clearly visualized in the picture:
- Narrowing of the common gap;
- Change the contours of the contact bones;
- disturbed bone structure in the affected area;
- Bone growth (osteophytes);
- Craumatic of the axis of the limb or finger;
- Subbluxation of the joint.
You can be prescribed for more detailed diagnostics:
- Computer tomography (CT);
- Magnetic resonance imaging (MRI);
- Ultrasound of the joint;
- Arthroscopy (internal examination of the joint cave using a camera that is introduced by a small puncture);
- Scintigraphy (evaluation of the condition of the bones and the metabolism by introducing radiopharmaceutical drugs).
In the event of a suspicion of the secondary nature of the disease, suitable tests and consultations of close specialists are prescribed.
Treatment of the arthrosis of the joints
The choice of the methodology for the treatment of osteoarthritis of the joints depends on the cause of the disease, its stages and symptoms.In the arsenal of doctors there is:
- Drugs;
- Not -drug treatment;
- Surgical methods.
In addition, the patient must strictly observe a diet and adapt his lifestyle to minimize further damage to the joints.
Drug treatment
The appointment of drugs for osteoarthritis follows two main goals:
- Distance of pain and inflammation;
- Restoration of cartilage tissue or at least stop the further degeneration.
Different types of medication are used to facilitate the patient's condition:
- Non -steroids anti -inflammatory medication in the form of tablets, injections, ointments or candles;They relieve pain and inflammation well;
- Hormones (corticosteroids): shown in severe pain and mostly inserted directly into the joint cavity;
- Other analgesics, for example anti -spasmodic effect: reduce the level of pain by relaxing the muscles;
It is important to note: All types of painkillers are only used to facilitate the patient's condition.They do not influence the condition of the cartilage and accelerate its destruction with longer use and cause serious side effects.
The main preparations for the restoration of joints today are chondroprotectors.They contribute to the satiety of cartilage with nutrients, stop the monument and start cell growth processes.Means only have an early and average stage of developing the disease and are regularly subject to the long term.
Preparations that improve the microcirculation in tissues and anti -characteristics help to improve the effect of chondroprotectors.The former ensures a good supply of the affected area with oxygen and nutrients, and the latter slows down the processes of tissue destruction.
The selection of specific medicines, their dosage and the administrative regime are active in the doctor.
Not -drug treatment
Not -drug treatment includes the following methods:
- Physiotherapy:
- Shock wave therapy: destroys bone growth and stimulates blood circulation due to the effects of ultrasound;
- Automated electromostimulation: Exposure to electrical impulses to stimulate muscle contraction;
- Ultrafonophoresis: The effect of ultrasound in combination using medication;
- Ozonotherapy: introduction of a special gas mixture into the joint capsule;
- Physiotherapy sports lessons;
- Mechanotherapy: training therapy using simulators;
- Joint traffic to reduce the load;
- Massage.
Surgical treatment
Most Often, The Help of a Surgeon Is Required at the Severe Stails of the Disease.Depending on the localization of the pathological process and the degree of the lesion, it can be prescribed:
- Point: a puncture of the joint with the removal of part of the liquid and according to the administration of medicinal products;
- Correction osteotomy: removal of the bone, followed by fixation from a different angle to remove the load from the connection;
- Endoprosthetics: replacing the damaged connection with a prosthesis;Used in extremely neglected cases.
Arthrosis in children
Osteoarthritis is seen as a disease of older people, but can also be found in children.The most common cause of the pathology is:
- Congenital pathology of the connective tissue;
- serious injuries;
- Inheritance;
- Metabolic disorders and the work of the glands of internal secretion;
- Orthopedic disorders (flat feet, scoliosis, etc.);
- Obesity.
The arthrosis of the children is rarely accompanied by pronounced symptoms: the pain hurts and there is practically no stiffness and restriction of the function.Monothetic changes are found on an X -ray, an MRI and an ultrasound.The same products are used in treatment as in adults.Maximum attention is paid for the exercise of therapy and physiotherapy because they are particularly effective at a young age.Without treatment, the disease will sooner or later enter into the advanced stage with a complete loss of mobility.
diet
Nutrition is one of the most important factors in the treatment of osteoarthritis.In the presence of overweight, it is necessary to reduce it to reduce the load on the joints.In this case, a balanced diet with a lack of calorie is prescribed.Regardless of the body mass index, doctors recommend giving up fully:
- Fast carbohydrates (sugar, desserts, flour);
- Alcohol;
- Spices;
- Legumes;
- Strong tea and coffee;
- Excessively greasy and sharp dishes.
Provisions and post -hall are not excluded, but significantly limited and salt.Ideal nutrition for osteoarthritis includes:
- low -fat meat;
- Fish and seafood;
- Eggs;
- Dairy products;
- Linseed and olive vegetable oils;
- Vegetables and fruits, a large number of greens;
- Moderate muesli, pasta of hard -wrap pasta;
- Products with a high collagen content (jelly, watering, jelly).
prevention
Osteoarthritis is easier to warn than to treat.In order to maintain common health for many years, it is recommended:
- lead an active lifestyle;
- Train regularly and visit the pool;
- Eat properly, use enough omega-3 and collagen;
- prevent the BMI from exceeding;
- Wear comfortable shoes.
If the disease is diagnosed early, it is recommended to regularly undergo wellness treatment and to exclude professional risk factors: long -term stay on the feet, lifting of severity, vibration.
Consequences and complications
Osteoarthritis is going very slowly.When carrying out a doctor's bond, its electricity slows down significantly, so that you can maintain the joint mobility for much longer.Unreversible consequences develop without treatment:
- pronounced common deformation;
- Acceptance of mobility up to its complete loss (ankylose);
- Shortening the limb (with damage to knee or thigh connections);
- Deformation of bones, curvature of the limbs and fingers.
forecast
The forecast for osteoarthritis depends on the shape of the disease, its extent and treatment.Pathology is one of the frequent causes of disabilities and in advanced cases the ability to move and serve yourself.In the event of severe forms of damage to the knee and hip joint, the patient receives the first or second group of disabled people (depending on the level and the volume of the damage).
























